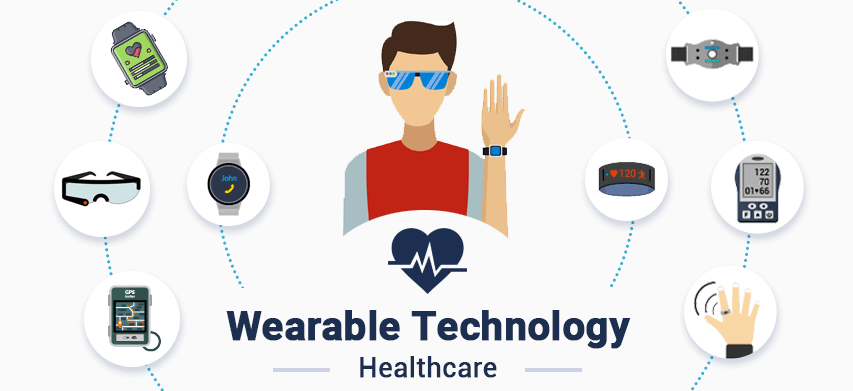
The COVID-19 pandemic strained healthcare facilities as infection rates rose. IoT solutions combined with wearable devices can enable remote monitoring of patient health and automation within healthcare facilities, reducing frontline exposure and workload.
Vital signs monitoring
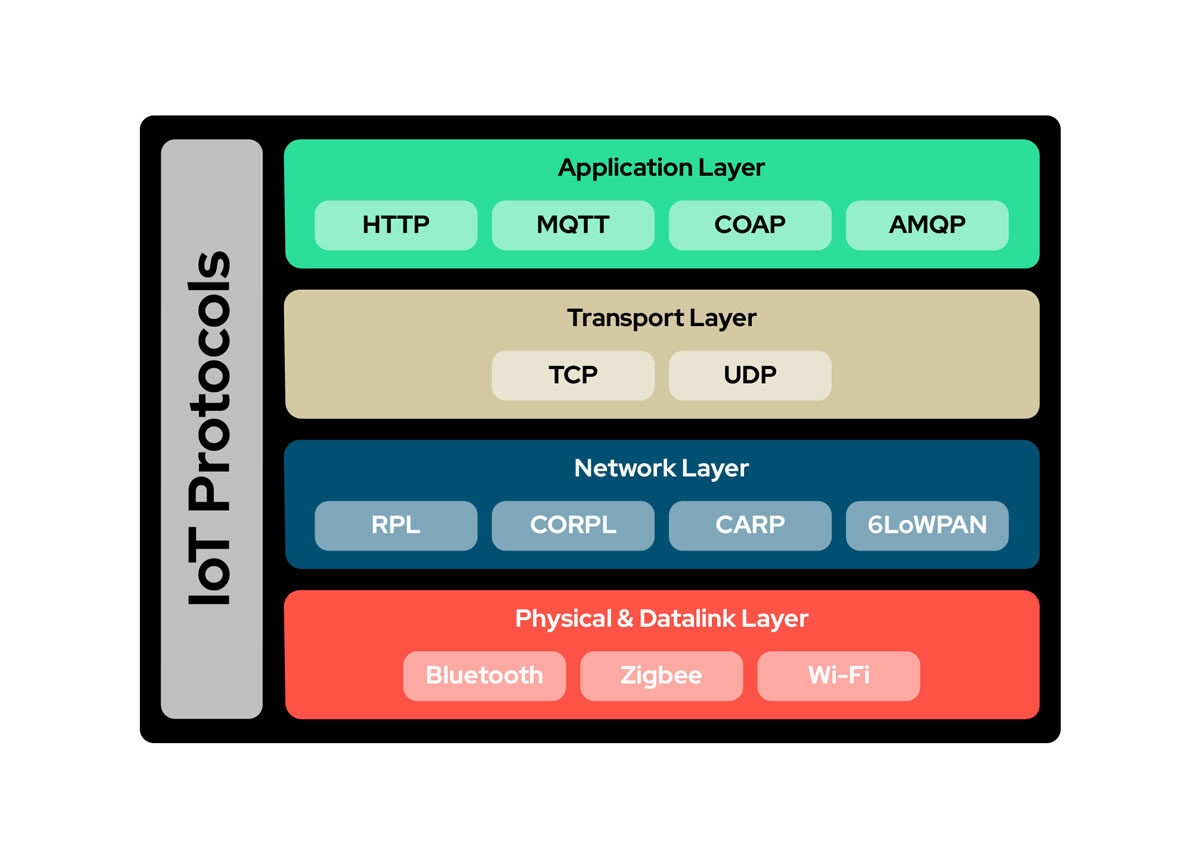
Frequent monitoring of patient vital signs is part of treatment. Direct contact between healthcare workers and patients increases the risk of virus exposure. Wearable integrated IoT solutions can capture key readings such as temperature, respiratory rate, blood pressure, pulse rate, and blood glucose. Devices can send readings at predefined intervals via Bluetooth, Zigbee, or other communication protocols to a Wi-Fi-enabled gateway device. The gateway can forward readings to the cloud, where analytics and machine learning can process the data and alert the nurse station if a patient's condition requires attention.
Activity tracking
COVID-19 wards are often isolated from other parts of a facility to reduce transmission. Patients sometimes attempt to leave isolation. Wearables can track patient activity in isolation wards without manual surveillance. If a COVID-19 positive patient attempts to leave, a wearable can provide location coordinates to the cloud so the system can notify the nurse station. Wearables can also warn nearby devices about the presence of a COVID-19 patient.
Staff screening
Guidelines recommend recording temperature readings for anyone accessing an operational site before allowing entry. For healthcare staff, regular temperature monitoring while on-site is important. Wearables can periodically record staff temperatures and transmit them to the cloud. The cloud can analyze the data and notify the nurse station if any staff member's temperature exceeds 37.4°C so the staff member can be isolated promptly.
Crowd monitoring
Social distancing guidelines recommend maintaining at least 2 meters from others and avoiding gatherings. Wearables can calculate distance to other devices and alert the wearer. Wearables can also update location coordinates to the cloud via gateway devices. The cloud can analyze uploaded coordinates and notify administrators when crowding occurs in parts of a facility so managers can clear congested areas and enforce distancing.
Contact tracing
Contact tracing is a public health tool to break transmission chains and is critical in healthcare settings because admitted patients often have weakened immune systems and elevated infection risk. Wearables can assist contact tracing if any staff member tests positive for COVID-19, helping to interrupt transmission chains.
Medication schedules
Rising patient numbers and staff shortages increase the burden of tracking medication schedules, injections, and dosing times. Wearables can be programmed with medical chart details and medication schedules to reduce this burden. Wearables can also remind patients to take medication on time, which helps maintain consistent drug levels and can aid recovery.
Disinfection schedules
Maintaining disinfection of indoor and outdoor areas is a recommended prevention measure. Healthcare facilities should disinfect regularly to protect patient safety. Wearables can be programmed with disinfection schedules to ensure comprehensive and regular cleaning without disrupting operations.
Beyond these use cases, wearables have many other applications in healthcare facilities, personal care, and fitness. The following summarizes key development challenges and possible approaches:
Data security and privacy
One major risk of IoT solutions is data security and privacy, since they capture, transmit, and store sensitive vital signs and patient health records, commonly referred to as PHI (personal health information) among solution components. Cybercriminals can exploit IoT systems and misuse PHI to create fraudulent insurance claims or purchase medication. IoT solutions should comply with HIPPA standards, a U.S. statute intended to set national standards for protecting PHI held or transmitted in electronic form. Integrated secure communication protocols and encryption mechanisms should be used to protect PHI in transit and at rest.
Interoperability issues
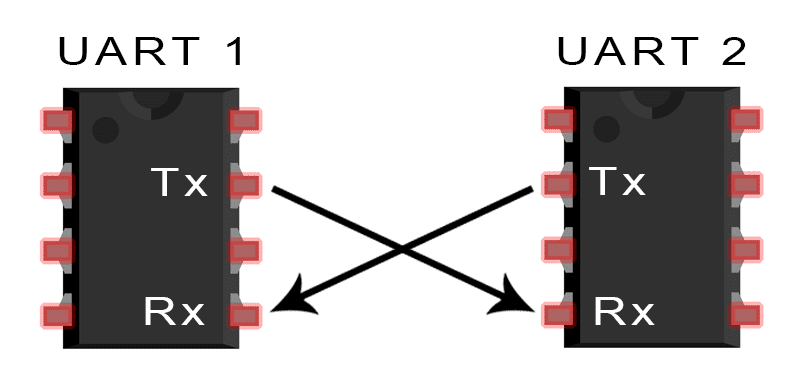
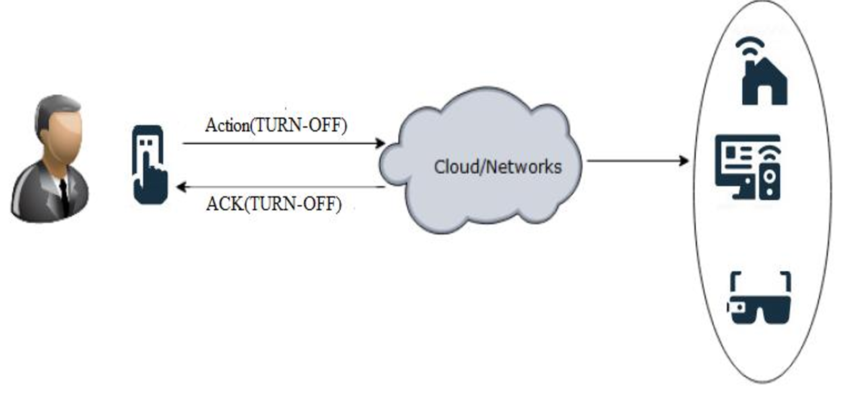
Integrating various IoT devices in healthcare is challenging because each vendor may support proprietary or different communication protocols and data formats. Devices from different manufacturers may not communicate effectively if standards are not agreed. IoT device architectures should be flexible enough to support multiple communication protocols and authentication mechanisms. Support for multiple data formats is also important to ensure easy integration with various cloud services.
Large-scale data collection
Sensors used for patient vital sign monitoring generate continuous streams of data that must be stored in the cloud, which can drive up storage costs and complicate decision-making during care. IoT systems should be designed with appropriate data-driven learning techniques that extract useful subsets of data for storage and processing, reducing cost and aiding decisions. Edge-capable IoT devices should also be able to perform local processing to filter or summarize raw data, saving upload bandwidth and cloud processing.
 ALLPCB
ALLPCB